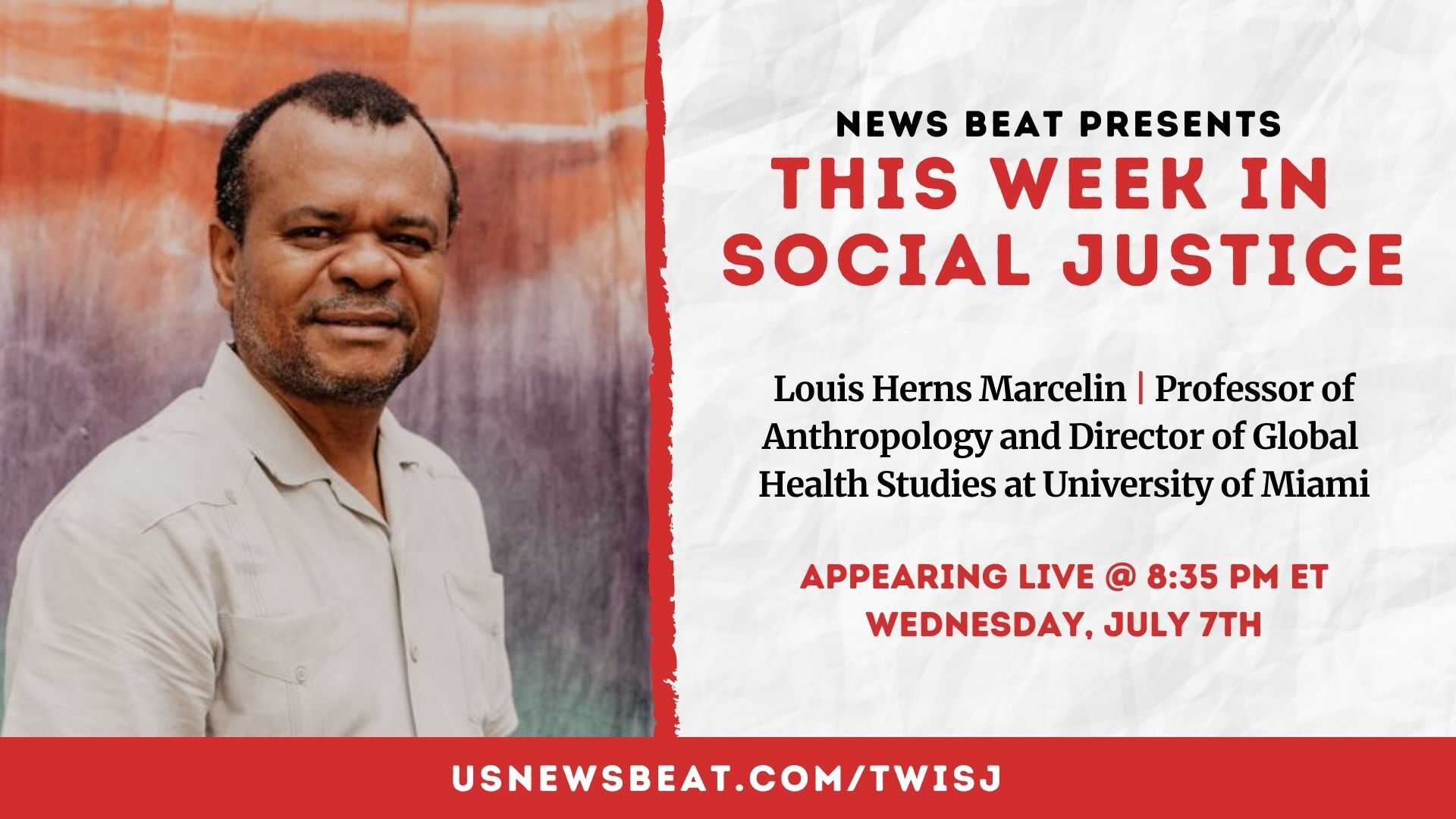
Listen to this special bonus episode exploring the threat the coronavirus poses to jails and prisons throughout the United States. Subscribe to News Beat podcast on your favorite pod app here.
One of the foremost experts on correctional health services warned of a “very perilous and looming threat” inside American correctional facilities amid the coronavirus pandemic outbreak.
The warnings from Dr. Homer Venters, an epidemiologist, and former chief medical officer for New York City’s jails, comes as public health officials and prison reform advocates express concern over already insufficient healthcare services inside jails and prisons throughout the United States, which has the highest incarceration rate in the world.
For weeks, health officials have sounded the alarm over the rapidly spreading coronavirus, also known as COVID-19. It has infected more than 130,000 people globally and has killed more than 5,000. President Donald Trump declared a state of emergency on Friday, just days after the World Health Organization (WHO) characterized the coronavirus as a pandemic.
The infectious disease has upended daily life of people across the globe—and experts in the United States say it’s unlikely jails and prisons will be spared.
“These places also have chronic understaffing of security staff and health staff,” Venters, president of the nonprofit Community Oriented Correctional Health Services and author of “Life and Death Inside Rikers Island,” tells News Beat podcast. “And so many of the ways in which these buildings and places are designed and run promotes the spread of communicable disease. And then we have health systems in these places that will be trying to prepare for this outbreak.
"But those are not health systems that are run by or even really connected with the kind of health systems that we're used to in the community that uses basic standards of infection control, and even data reporting and transparency about who's getting tested," Venters continues. "And so I have grave concerns about the patients and that's really the most important part of this.”

(Caption: Dr. Homer Venters, former chief medical officer of New York City's jails, including Rikers Island.)
There are more than 2.2 million people behind bars in the United States, disproportionately African American. One reason for the prison surge in recent decades is punitive sentencing laws passed in the late 1980s and early 1990s. Of the entire world prison population, 40 percent of people serving life sentences are in the United States—meaning America is also home to a large percentage of aging inmates.
RELATED: DR. HOMER VENTERS DISCUSSES MENTAL ILLNESSES IN JAILS AND PRISONS
RELATED: READ OUR SERIES ON MASS INCARCERATION AND DOWNLOAD A SPECIAL CRIMINAL JUSTICE SPOTIFY PLAYLIST
According to a Bureau of Justice Statistics (BJS) report published in 2015, half of state and federal prisoners reporting having experienced a chronic condition, such as cancer, high blood pressure, health-related problems, and diabetes, among others. Older prisoners were three times more likely to report such conditions, the BJS found.
The Pew Charitable Trusts in 2018 reported that imprisoned inmates increased 280 percent between 1999 and 2016, while the growth of younger prisoners was 3 percent. That America’s prisoners are increasingly aging is significant considering seniors are most vulnerable to the coronavirus.
“We've filled up our jails and prisons with people who are disproportionately people of color, but also people with serious physical and behavioral health problems,” Venters says. “So people who are at high risk and the push of mass incarceration from the '80s, and '90s, and 2000s means that we have many older patients in these places, too. So it really is a confluence of worst possible scenarios. And we have people working in these places and detained in these places that are looking at really a very perilous and looming threat.”
Weeks into the outbreak in the United States, experts have called on increased guidance from public officials and for reducing the number of bail-related jail admissions.
“[P]olicing patterns should not continue at the status quo,” experts wrote in the journal HealthAffairs. “Bringing more people into the correctional setting during this period creates additional risk. In the absence of more comprehensive judicial reform, law enforcement agents can consider limiting further incarceration to egregious crimes rather than populating our jails and prisons with individuals convicted of non-violent crimes.
Prison Policy Initiative, which advocates for prison reform, urged officials to release vulnerable prisoners suffering from chronic illnesses, reduce jail admission, and suspend medical co-pays inside prisons.
Meanwhile, Venters issued this stark warning:
"My concern is that we'll have many preventable deaths, because we haven't figured out how to find the people who are sick in these settings and get them to inpatient care," he says. "And it doesn't just impact them and their families. It also means that you have untreated serious infection, in this case a communicable disease, still sitting in one of these buildings."
To learn more about healthcare inside jails and prisons and the implications of a coronavirus outbreak inside these facilities, listen to the special bonus episode or read the full transcript below, which has been edited for clarity.
TRANSCRIPT
News Beat: Dr. Venters, before we get into the coronavirus outbreak, can you just give listeners a general idea of what healthcare services are like in U.S. jails and prisons?
Dr. Homer Venters: Healthcare services behind bars are generally substandard and disconnected from all the basic institutions that promote quality and transparency in the rest of our nation. So the bodies that we're hearing about every day, the CDC or state department's of health, local departments of health, they're really outside the walls of these places. And so most health care services behind bars are run by security services, by sheriffs and commissioners of correction. And they're the ones that we've left with a job of figuring out what's the right amount of quality, the scope of services and the transparency, and so as you can imagine, they're not healthcare professionals and they have not been able to establish any kind of clinical standard of care behind bars. So the status is quite poor, and it's quite removed from our eyes.
NB: We’re already at a curious point where there are issues long-standing issues inside these facilities. So can you talk about how vulnerable these jails and prisons are to an infectious disease outbreak such as COVID-19? And in your response, if you can, can you talk about how jails responded to the H1N1 outbreak about a decade ago and what leaders can learn from that?
HV: Yes, the H1N1 was a really pivotal moment for us in outbreak response behind bars. I had the good fortune at the time, while I was working in Rikers Island, I was part of the Department of Health, which was managing the outbreak response for the entire community all of New York City. And so our team was just one part of the community's team, which is as it should be. Most jails and prisons, the health staff work for the sheriff or the commissioner of corrections and prison systems. What that means is those health services aren't integrated with outbreak response. And that's critically important because the places that people find themselves these jails and prisons, promote the spread of communicable disease, people are in very close contact, they often don't have access to basic hand-washing, they're very generally dirty and very poor, have poor infection control practices. These places also have chronic understaffing of security staff and health staff. And so many of the ways in which these buildings and places are designed and run, promotes the spread of communicable disease. And then we have health systems in these places that will be trying to prepare for this outbreak. But those are not health systems that are run by or even really connected with the kind of health systems that we're used to in the community that use basic standards of infection control, and even data reporting and transparency about who's getting tested. And so I have grave concerns about the patients and that's really the most important part of this. We've filled up our jails and prisons, with people who are disproportionately people of color, but also people with serious physical and behavioral health problems. So people who are at high risk and the push of mass incarceration from the '80s, and '90s, and 2000s means that we have many older patients in these places, too. So it really is a confluence of worst possible scenarios. And we have people working in these places and detained in these places that are looking at really a very perilous and looming threat.
NB: We spoke to you before for an episode on mental health and incarceration, and you talked about this fundamental disconnect between security staff, the correctional officers, and the medical service providers. So on the most basic level, how can jails and prisons effectively communicate a response to take on this enormous challenge?
HV: I think that the institutions that are directing the community responses in these settings, that means the local departments of health, the state department's of health, they need to integrate correctional administrators, security staff and the correctional health staff together. Because it is clear that these places do not have the resources. Even managing the inside-the-jail or inside-the-prison response requires tremendous amounts of help from the outside. So most of these places right now have to beg, borrow or steal just to get testing kits, for instance, they don't have testing kits, so they have to go ask for them every time they need one. Getting hospital access to hospital beds, for patients who become ill in these places, is not an easy task. Many hospitals may balk at the idea of multiple patients coming in who are sick from a jail or prison, who each of them is accompanied by two correctional officers. But all we must be unambiguous right now that access to all the levels of testing and care must be available based on clinical needs, not based on criminal justice status. And I fear that without integrating the managers and administrators and people who are experiencing these incarceration right now, if they're not in the room when we're deciding these local and state policies, they're going to be left out just as they have all along the way before.
NB: Dr. Venters, you mentioned before the prison and jail boom several decades ago. And as you know, in the 90s and even in the late 80s, we had these state and federal officials pass enhanced sentencing laws that just put people in jails for longer and longer. And there was a study that was done that said the number of people 55 or older in state and federal prisons increased 280% between 1999 and 2016. So as we know, seniors in the general population are most vulnerable to COVID-19. So how can this particular jail population be protected?
HV: Well, this is a really vexing problem because when H1N1 hit it was the inverse, right? We have lots of young patients, adolescent patients being affected. And so it was very, even with that response, it was very complicated to figure out, how do we come up with special housing areas for people to be held in, the sick people are in one spot, the well people in another spot, we have differences between who has symptoms and then who has symptoms and also has been diagnosed. And then how do we get the sickest people to the hospital. All of that was difficult, but just with dealing with one subset. The patients who are older are dispersed throughout all the parts, all the security classifications, all the types of housing areas, in these jails and prisons, and it is no small feat to think about how would we -- for those of them that develop some symptoms, we would want them in a specialized housing area. Well, if some of them in a jail, for instance, are pre-trial, and some of them have been sentenced, or if some of them are higher security classification and lower, it doesn't take much to understand that this presents a very difficult management task for the jail or prison administrators. Then if you add in the fact that many of these patients need test kits and testing and then they need access to hospitals, if they become sick. And really, this is also made worse by the fact that most jails and prisons don't have good data systems. So today, every jail and prison you would expect, knows who are the patients who are at high risk, who are the older patients, who are the patient's with chronic medical problems, but in prisons and jails that operate with paper medical records, which many of them still do, they have to go through rafts of either Excel spreadsheets used to track diabetics and put that together with asthma encounters and look through paper charge. And remember that these criteria may change day to day; what we knew last week about this virus is different than what we know today. So the lack of capacity to operate on a population health level, that is to look at risk management and who are the patients at high risk, how do we manage them day to day, this will be very difficult for these places, both because of the physical plant management, also, because of the data systems that are needed to find and care for the sickest patients or the patients at highest risk. So it will be a tremendous challenge in these places. And then, you know, still my primary concern is that when patients develop symptoms and become sick, that they be afforded the same level and standard of care that's available in the community and our experience in lots of other instances is that will be an uphill climb. Both because these places aren't built for transparency. So families and local officials may not find out that people are sick right away. And, you know, unlike a school which sends out a report every day -- we have a test that's positive or this is what we're doing -- that ethos of transparency, will I fear stop at the walls of these places, unfortunately.
NB: One other issue that you're bringing up is the lack is testing. And as we know, in the United States, we are falling behind in terms of testing for this disease. There has been I think, as of today, maybe up to 10,000 people officially tested in the country, and other nations have tested a lot more people. Are you concerned that jails and prisons won't be prioritized in terms of testing if there are doctors on the outside who can't even get this test for the patients that are coming to see them?
HV: Absolutely, I'm concerned. As you think about the different large domains of work, there's surveillance to find who are the people are at risk, and then there's active surveillance that'll probably happen with people who develop symptoms, and then that will involve testing. We have to have an unambiguous standard that's based on clinical need, and promoting clinical outcomes, like saving people's lives, and that is the job of the local commissioners of health, state commissioners of health, state department's of health, and the CDC, to be very clear that these standards don't stop at the walls of jails and prisons. And so the person who meets clinical criteria for a test, must be given a test and they shouldn't be denied the test or inpatient care or access to a ventilator and respiratory technicians because of their criminal justice status and. Our experience with many other responses is that that discrimination will creep in, and so we have to be very vigilant about it. The thing we have today that we didn't have 10 years ago is we have this really incredibly active network of activists of groups with lived experience like Just Leadership, investigative reporters like yourselves who are looking for these things. I've been actually quite surprised and pleased with the amount of interest in the potential plight of people behind bars. So it doesn't mean that these institutions are any better than they were 10 years ago. But the fact that we can hold officials to account quickly, to say, look, if you're testing people in the community, and if you say that you have housing areas that you're isolating because some people have some flu symptoms, why aren't you testing those people? What's your ethical and, and clinical rationale for denying people access to that care?
NB: In terms of recommendations, so as we know, there are thousands of people that are going in and out of jails and prisons each day in America. We've had significant criminal justice reform, especially surrounding the issue of bail. So potentially there are less people going in on a daily basis. So what policies need to be made on the outside in terms of talking with prosecutors and local police departments about potentially putting less people in jail during this time period to prevent an outbreak?
HV: Well, I think ironically, I don't know if it's ironic, but I think one of the most important voices in this discussion are especially county sheriffs. They look at their facilities right now and I've talked to sheriffs and their staff all over the country who are terrified about the prospect of you know if they right now have a jail, a county jail that is 70-80% full, they have already thought through more than most of us would even understand how difficult it will be for them to manage this outbreak. Their voices actually are really important to get forward because these are not people that are shy about promoting public safety as the top priority. But their inability to do just basic, competent outbreak management should help us rethink all of the earlier steps. The other part of this, thinking about certainly diversion alternatives, this is a critical time to maximize those opportunities. But we should also recall that with H1N1, there were patients who were in jail who couldn't get out because they didn't have access to the courts. And so just as correctional staff will get sick and teachers will get sick and doctors will get sick, correctional officers are going to get sick but also judges and prosecutors and defense attorneys, and so we have the experience during H1N1 that there were people in jail that were still in jail because they couldn't access the courts for one reason or another and this will happen all over the country. And not just for county jails. Think about if you had a hearing in immigration detention and you need to go for some sort of hearing, that was your path out of the building, prison also. Many of these administrative processes, they'll be affected just like every other part of our community. So the less full these buildings are when the virus hits the building, the more likely we are to avoid what are going to be I think preventable deaths.
NB: Dr. Venters, I don't want to sound like an alarmist, but this does feel like it's still we're in the beginning stages of this outbreak in the United States. You could correct me if I'm wrong, you have more experience. With that being said, what is the sort of worst-case scenario in your mind if there is an outbreak in a particular jail or prison or multiple facilities in this country?
HV: Yeah, I think that, you know, we hear, it's interesting al the terms of art that Americans have and people all over the world have learned in the last two weeks. You know, we've heard a lot about infection control about the importance of hand-washing, social distancing is something that we talk about all the time now. Those are really things that are inaccessible to most people behind bars. So many people behind bars don't really have access to hand-washing when they want to; if you're in an intake pen, if you're in a housing area with 40 people, and there's one sink that works and no soap, which is pretty standard from the places I've seen around the country, those things and the ability to distance yourself from the people around you, that's not possible. And all of this is important because another term we hear a lot about is flattening the curve. And so that's this notion that we're in the beginning of an outbreak, as you just said, it's a pandemic. And so we're in this kind of exponential rise, the curve is going up, right, we're having more and more cases every day as we track it along, day by day by day. So all of these measures about social distancing and closing schools, things like this are really effective measures to flatten that curve, that is to slow the rate of rise of new cases. We already know that people who are behind bars face barriers and access in inpatient care, hospital care. And that's really critical when we talk about flattening this curve. We're trying to not overwhelm the hospital system, especially for inpatient hospitalization of people who need it, who have coronavirus and are sick. for patients behind bars who already face barriers to make that step. My concern is that we'll have many preventable deaths, because we haven't figured out how to find the people who are sick in these settings and get them to inpatient care, and it doesn't just impact them and their families. It also means that you have untreated serious infection in this case a communicable disease still sitting in one of these buildings. And so that is my concern and my fear is that we have preventable deaths happening disproportionately among people who are incarcerated, people of color, and also that these places could quickly slip into chaos when correctional staff are sick, the health staff are sick and the chronic misinformation and and rumor mill that happens in every jail in prison takes over.
NB: Since you mentioned it -- that more people are seemingly having this conversation about infectious diseases inside jails and prisons than they would have going back several years even back to each one and one. Can you just inform listeners about some other important steps that you'd like to see jails and prisons take going forward regardless of an infectious disease outbreak? What can be done to improve health care inside these facilities? I know that it's probably a long list, but are there some key things that could be done to improve the situation?
HV: Sure, it is a big lift because we spent decades building this siloed and inadequate health system. I think that the, you know, the CDC, the Centers for Disease Control, should have an office of detention or correctional health and that should be monitoring all health outcomes in these places, not just infectious or communicable disease, but traumatic brain injury that occurs behind bars, access to health and health outcomes in those places. State department's of health and county departments of health should have a role in determining what's good quality health care and all these places. We shouldn't leave that to commissioners of correction and sheriffs. And finally, at a higher level, you know, we should eliminate the inmate exception of the Social Security Act of 1965. That's the law that precludes the use of Medicaid funds behind bars or federal funds for institutionalized people and while it keeps fun those funds out, it also keeps those quality metrics out. So all of those are kind of our public institutions to promote health quality. They should be applied inside these places. Because as we find out now, these places are part of the community, but we are about and the people who are incarcerated are about to pay the price for having pretended that they aren't.



.jpg)